Strokes affect 800,000 people in the U.S. each year at a cost of $34 billion, according to the CDC. [1] It is the leading cause of serious long-term disability and extreme reduction in mobility,[2] as well as the second leading cause of dementia.[1]
Each minute is crucial when diagnosing a stroke, and advocacy groups work to educate the public on the signs and symptoms of stroke so patients can be treated as quickly as possible. Stroke guidelines recommend interpreting CT scans within 45 minutes of a patient arriving in the ED. This goal is difficult to meet if a hospital does not have access to a stroke specialist.[2] Only 55% of Americans have access to stroke centers within a 60-minute drive. Almost half of those hospitals with stroke centers have fewer than 100 beds and no staff neurologist.[3]
With time to treatment vital to patient survival, access to telestroke services could save lives and improve outcomes.
Telestroke Explained
A telestroke program allows for two-way communication between a hospital’s on-call neurologist and a community hospital’s ED physician to effectively treat and diagnose patients presenting with symptoms of a stroke. These programs decrease time to treatment and the need to transport patients.[1]
Telestroke programs utilize a hub-and-spoke model to provide care to community hospitals that don’t have the same access as a heavily resourced larger hospital. They deliver expertise to hospitals that lack an on-call neurologist to properly and efficiently diagnose and treat stroke victims. 80% of strokes are ischemic strokes.[4] When a patient presents at the ED with this type of stroke, it is critical that tissue plasminogen activator (tPA) is administered within four hours of a stroke. A Kaiser Permanente study found there was a 75% increase in timely use of tPA when telestroke was utilized, compared with cases when telestroke is not utilized. This study found that unwarranted clinical variation could be almost eliminated by utilizing a standardized telestroke program in hospitals that lack access to a full-time, on-call neurologist as well.[7]
Telestroke services also can reduce the length of time a patient needs to be hospitalized. For example, Southern Illinois Healthcare consists of a group of small, community hospitals. Once the system implemented a telestroke program, they were able to reduce the average length of stay for stroke patients by 2.5 days.[5]
The FAST Act Changes
The FAST (Further Access to Stroke Telemedicine) Act was signed into law in February 2018 in the Bipartisan Budget Act, mandating that effective January 2021 Medicare reimburses telestroke services regardless of where patients receive treatment.[1]
Currently, Medicare reimburses telestroke services just for patients in rural areas. Because only 6% of all strokes occur in rural areas, the vast majority of strokes occur in regions where Medicare currently does not reimburse telestroke services.[2]
This FAST Act will allow stroke victims to gain access to high-quality care through telestroke services, regardless of their location. ED physicians in community hospitals can work with on-call neurologists to provide appropriate, high-quality care in a more efficient and cost-effective manner.
There has been a reluctance to implement telestroke services in community hospitals due to the location, reimbursement limitations, and the high upfront costs. Implementing a telestroke service can have an upfront cost between $10,000 and $100,000, but the annual maintenance cost is likely less than $10,000.[6]
Impacts of the FAST Act
Ensuring telestroke services are reimbursable under Medicare will allow for increased access to neurology services. Additionally, fewer complications and disabilities from delayed stroke treatment will decrease the need for funds from the federal government.[7] The biggest benefits of telestroke services are:
- Increased patient access: Staffing pressures are decreased for facilities amid a neurologist shortage.
- Improved outcomes: Compared with a patient in a small, community hospital receiving routine care, a patient receiving telestroke services has an average expected lifetime cost savings of $1,436 (due to a decreased need for long-term care) and gain 0.02 QALYs.[8]
- Further telestroke adoption: Given increased reimbursement levels, more facilities are projected to invest in telestroke services.[9]
Considerations for Incorporating Telestroke Services
Adopting telestroke services can change the way your facility will utilize telehealth, especially if you are in a suburban, community hospital. It will increase access to improved stroke care for patients, no matter their location. Additionally, it allows the flexibility to use a telestroke program instead of having a full-time, on-call neurologist at each emergency department, potentially saving costs for these facilities.
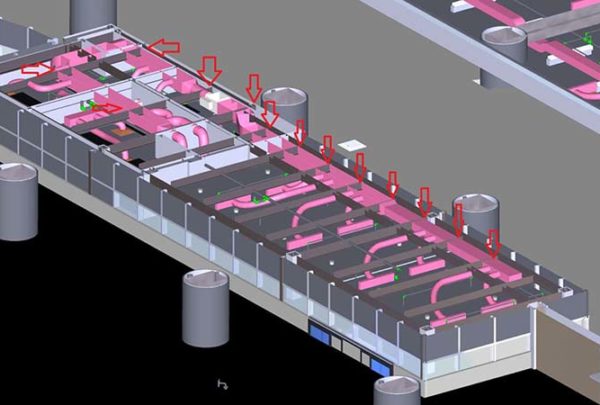
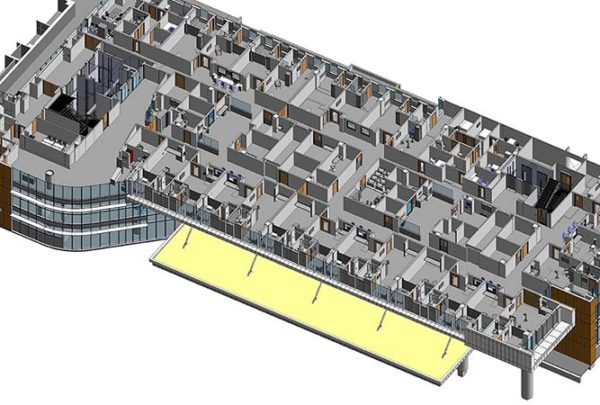
When planning for future facilities, it is crucial that technology and adaptability are available for health centers to adopt these lifesaving telestroke services.
Healthcare systems must ensure that their EDs are technologically capable of running a telestroke program.
Successfully integrating a telestroke program into your facility can be a life-saver to your patients, improving their outcomes and reducing treatment costs.
[1] “Telemedicine for Stroke Expanded with Passage of Fast Act. American Academy of Neurology Publications. Feb. 9, 2018. https://www.aan.com/PressRoom/Home/PressRelease/1618
[2] Peccim, Alexandra Wilson, “Medicare to Reimburse for Telestroke Regardless of Location”. HealthLeaders. Feb. 20, 2018. https://www.healthleadersmedia.com/innovation/medicare-reimburse-telestroke-regardless-location?page=0%2C1
[3] Bladin M.D., Christopher, Cadilhac, PhD, Dominque, “Effect of Telestroke on Emergent Stroke Care and Stroke Outcomes”. American Heart Association Journals. March 25, 2014. https://www.ahajournals.org/doi/pdf/10.1161/STROKEAHA.114.003825
[4] “About Telestroke”. Partners Telestroke Center: Massachusetts General Hospital and Brigham and Women’s Hospital. https://telestroke.massgeneral.org/telestroke.aspx
[5] O’Dirdan, Beth, “Improving Stroke Patient Outcomes with Telestroke Programs”, American Well, Sept. 12, 2018. https://www.americanwell.com/improving-outcomes-telestroke/
[6] “Neuroscience Technology Compendium: Technology Trends Overview”. Advisory Board. November 2017. https://www.advisory.com/-/media/Advisory-com/Research/SLSA/Resources/2017/Technology-Compendiums/2017-Neurosciences-Technology-Compendium.pdf#page=13
[7] Wicklund, Eric, “Telemedicine-Friendly FAST Act Heads Back to Congress”. mHealth Intelligence. Feb. 17, 2017. https://mhealthintelligence.com/news/telemedicine-friendly-fast-act-heads-back-to-congress
[8] Veigh, Jim, “Mayo Clinic Researchers Show Telestroke is Cost-Saving. Mayo Clinic. Jan. 16, 2014. https://newsnetwork.mayoclinic.org/discussion/telestroke-is-cost-saving-for-society-mayo-clinic-researchers-show/
[9] Musco, Sarah, “Neurosciences Market Trends”. Advisory Board. Feb. 13, 2019. https://www.advisory.com/research/service-line-strategy-advisor/resources/2014/neurosciences-market-trends