Most hospital department leaders receive robust support, strategies, and tools to guide career transitions. Few, if any, receive the resources to navigate major construction and workflow re-engineering transitions. While redesigned space offers a chance for a fresh start, it also places the leader in a position of acute risk and vulnerability. They become the “lead point person” on a construction project without the requisite training. Further, this complex add-on responsibility competes with the demands of managing day-to-day department operations.
What is transition planning?
Transition planning orchestrates the physical, clinical, and operational logistics of moving into a space and includes:
- Transition budgeting
- Assembling the right teams and structure
- Collaborating with interfacing hospital departments and ancillary groups
- Staff and patient circulation
- Seamless IT service with minimal downtime
- Staff workflow training in new and interim configurations
- Clinical equipment: move vs. buy new, installation and de-installation, de-commission, acquisition and tagging, biomedical testing and sign off.
- Locations for supplies and how to restock them
- Testing new space and technology before occupancy
- Facility readiness for full functionality
- Planning for dual department operations, when needed, such as Emergency Department services
- Operational readiness and testing through clinical scenario analysis
- Issue tracking
- Contingency planning and risk mitigation
- Operations preparedness with updated policies, procedures and protocols
- Communication plan, PR, Welcome Brochure, downloadable maps, and virtual tours for patients and visitors.
- Intranet resources for staff wayfinding
- Hour-by-hour relocation schedule that ensures quality caregiving operations and safe movement of patients.
- External integration with community partners such as EMS, private providers, and discharge facilities
- Planned disaster response during and after a move
- Post-occupancy command center that manages issue resolution
- Evaluation process six months after occupancy
Transition planning covers a range of strategic and operational issues from pre-design through post-occupancy. Beyond “what, when, and where” move management logistics and phasing, good transition planning offers:
- Pre-move task schedules and checklists,
- Staff training and orientation templates,
- Issue tracking, and,
- Common pitfalls with ways to avoid them.
It also engages staff in scenario drills to heighten anticipation and prepare for move and post-move days. Time spent in transition planning is the differentiator between existing in a new space and optimizing its performance.
Types of transitions
Depending upon the circumstances, hospitals may choose to transition in one or more ways:
Incremental implementation or phased approach
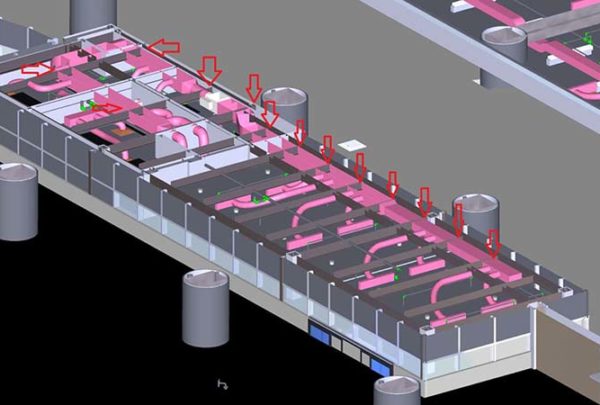
As an example, inpatient units typically transition in multiple phases by relocating small groups of patients from the existing space to new space. Or, in large renovation projects, new space may become operational first so that existing space can close for construction.
Parallel execution
It is not unusual for some healthcare services to conduct parallel operations for a period of time during a transition. This means redundant operations occur simultaneously in both the new space and the existing department. Examples may include emergency departments, medical imaging, and laboratory services. Parallel logistics are crucial when construction cannot disrupt 24/7 services.
One-time conversion and switchover
After business hours or over a weekend, it is possible to shut down some non-clinical support services in an existing space, relocating furnishings and equipment, and then resume operations in a new space. Administrative offices, switchboard communications, medical records, and food services may use this approach, as do scheduled clinical services such as sleep study labs and endoscopy procedures.
When should transition planning start?
Hospitals that treat go-live transitions as one-time events miss out on opportunities to boost long-term value and results. The mission of transition planning is to help users comprehend how the new space optimizes work long before occupancy. Moving day is simply the opening performance after many carefully orchestrated rehearsals.
In an ideal world, transition planning begins eighteen months before relocation. By doing so, the transition plan can inform the design and dovetail with the construction process. Such synergies enable the team to capitalize upon opportunities to improve patient care.
In Part 2 of this series, we cover what constitutes a successful transition and different ways to distribute the workload.